 1. J Health Care Mark. 1993 Fall;13(3):60-5.
1. J Health Care Mark. 1993 Fall;13(3):60-5.
Patient callback program: a quality improvement, customer service, and marketing tool.
Gombeski WR Jr(1), Miller PJ, Hahn JH, Gillette CM, Belinson JL, Bravo LN, Curry
PS.
Author information:
(1)Cleveland Clinic Foundation, OH.
The authors developed, implemented, and evaluated a callback program in which
hospital patients are contacted three weeks after discharge to resolve clinical
or service concerns. Of the more than 2,000 patients contacted during the
initial pilot test, 6% said they had a clinical concern and were promptly
directed to a physician’s office. A randomized/controlled study comparing a
control group of patients (who were not called) to an experimental group
(called) shows that several satisfaction measures increased positively within
the experimental group. The authors conclude that the Patient Callback Program
contributes to more effective clinical care and to perceptions of higher
customer service.
PMID: 10129817 [Indexed for MEDLINE]
2. J Low Genit Tract Dis. 2016 Jan;20(1):47-51. doi: 10.1097/LGT.0000000000000153.
Intimate Partner Violence and Barriers to Cervical Cancer Screening: A Gynecologic Oncology Fellow Research Network Study.
Levinson KL(1), Jernigan AM, Flocke SA, Tergas AI, Gunderson CC, Huh WK,
Wilkinson-Ryan I, Lawson PJ, Fader AN, Belinson JL.
Author information:
(1)1The Kelly Gynecologic Oncology Service, Department of Gynecology and
Obstetrics, Johns Hopkins Hospital, Baltimore, MD; 2Divsion of Gynecologic
Oncology, Women’s Health Institute, The Cleveland Clinic, Cleveland, OH;
3Department of Family Medicine and Epidemiology and Biostatistics, Case Western
Reserve University, Cleveland, OH; 4Department of Obstetrics and Gynecology,
Division of Gynecologic Oncology, Columbia University Medical Center, New York,
NY; 5Department of Obstetrics and Gynecology, Division of Gynecologic Oncology,
University of Oklahoma, Oklahoma City, OK; 6Department of Obstetrics and
Gynecology, Division of Gynecologic Oncology, University of Alabama at
Birmingham, Birmingham, AL; 7Department of Obstetrics and Gynecology, Division
of Gynecologic Oncology, Washington University, St. Louis, MO; and 8Preventive
Oncology International, Cleveland, OH.
OBJECTIVES: The aims of the study were to examine barriers to cervical cancer
screening among women who have experienced intimate partner violence (IPV) and
accessed domestic violence shelters, to compare barriers among those up-to-date
(UTD) and not UTD on screening, and to evaluate acceptability of human
papillomavirus self-sampling.
MATERIALS AND METHODS: This is a cross-sectional survey in which domestic
violence shelters in Ohio were identified and women completed an anonymous
survey assessing UTD screening status, barriers related to screening, history of
IPV, intention to follow up on abnormal screening, and acceptability of
self-sampling. Characteristics of UTD and not UTD women were compared using
Mann-Whitney U tests.
RESULTS: A total of 142 women from 11 shelters completed the survey.
Twenty-three percent of women were not UTD. Women who were not UTD reported more
access-related barriers (mean = 2.2 vs 1.8; p = .006). There was no difference
in reported IPV-related barriers between women who were not UTD and those who
are UTD (mean = 2.51 in not UTD vs 2.24 in UTD; p = .13). Regarding future
screening, of the women who expressed a preference, more women not UTD preferred
self-sampling than UTD women (32% vs 14%; p = .05).
CONCLUSIONS: In this study, access-related barriers were more commonly reported
among women not UTD with screening. Addressing these barriers at domestic
violence shelters may improve screening among not UTD women. Self-sampling may
also be one feasible approach to support screening in this population.
DOI: 10.1097/LGT.0000000000000153
PMCID: PMC4693628
PMID: 26704329 [Indexed for MEDLINE]
Conflict of interest statement: Conflict of Interest Statement: None of the
authors has any competing financial interests.
3. Cancer Epidemiol Biomarkers Prev. 2025 Jan 9;34(1):159-165. doi:
10.1158/1055-9965.EPI-24-0999.
A Mail-Based HPV Self-Collection Program to Increase Cervical Cancer Screening in Appalachia: Results of a Group Randomized Trial.
Reiter PL(1)(2), Shoben AB(1)(2), Cooper S(1), Ashcraft AM(3), McKim Mitchell
E(4), Dignan M(5), Cromo M(5), Walunis J(2), Flinner D(2), Boatman D(3)(6),
Hauser L(7), Ruffin MT 4th(8), Belinson JL(9)(10), Anderson RT(11)(12),
Kennedy-Rea S(3)(6), Paskett ED(1)(2)(13), Katz ML(1)(2).
Author information:
(1)College of Public Health, The Ohio State University, Columbus, Ohio.
(2)Comprehensive Cancer Center, The Ohio State University, Columbus, Ohio.
(3)School of Medicine, West Virginia University, Morgantown, West Virginia.
(4)School of Nursing, University of Virgnia, Charlottesville, Virginia.
(5)College of Medicine, University of Kentucky, Lexington, Kentucky.
(6)West Virginia University Cancer Institute, Morgantown, West Virginia.
(7)Cancer Center, University of Virginia, Charlottesville, Virginia.
(8)Family and Community Medicine, Penn State Health, Hershey, Pennsylvania.
(9)Preventive Oncology International, Inc., Shaker Heights, Ohio.
(10)Department of Obstetrics, Gynecology, and Reproductive Biology, Cleveland
Clinic, Cleveland, Ohio.
(11)Department of Public Health Sciences, University of Virginia,
Charlottesville, Virginia.
(12)School of Medicine, University of Virginia, Charlottesville, Virginia.
(13)Division of Cancer Prevention and Control, The Ohio State University,
Columbus, Ohio.
BACKGROUND: Despite the promise of mail-based human papillomavirus (HPV)
self-collection programs for increasing cervical cancer screening, few have been
evaluated in the United States. We report the results of a mail-based HPV
self-collection program for underscreened women living in Appalachia.
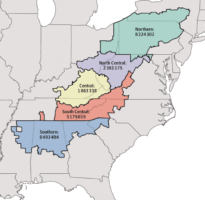
METHODS: We conducted a group randomized trial from 2021 to 2022 in the
Appalachian regions of Kentucky, Ohio, Virginia, and West Virgnia. Participants
were women of ages 30 to 64 years who were underscreened for cervical cancer and
from a participating health system. Participants in the intervention group (n =
464) were mailed an HPV self-collection kit followed by telephone-based patient
navigation (if needed), and participants in the usual care group (n = 338) were
mailed a reminder letter to get a clinic-based cervical cancer screening test.
Generalized linear mixed models compared cervical cancer screening between the
study groups.
RESULTS: Overall, 14.9% of participants in the intervention group and 5.0% of
participants in the usual care group were screened for cervical cancer. The
mail-based HPV self-collection intervention increased cervical cancer screening
compared with the usual care group (OR, 3.30; 95% confidence interval,
1.90-5.72; P = 0.005). One or more high-risk HPV types were detected in 10.5% of
the returned HPV self-collection kits. Among the participants in the
intervention group whom patient navigators attempted to contact, 44.2% were
successfully reached.
CONCLUSIONS: HPV self-collection increased cervical cancer screening, and future
efforts are needed to determine how to optimize such programs, including the
delivery of patient navigation services.
IMPACT: Mail-based HPV self-collection programs are a viable strategy for
increasing cervical cancer screening among underscreened women living in
Appalachia.
©2024 American Association for Cancer Research.
DOI: 10.1158/1055-9965.EPI-24-0999
PMCID: PMC11717618
PMID: 39445831 [Indexed for MEDLINE]
Conflict of interest statement: Dr. Belinson serves as a Medical Advisor to
Atila Biosystems. Dr. Paskett receives grant funding from Merck Foundation,
Genentech, Guardant Health, Astra Zeneca, and Pfizer for work not related to
this research. She is also an Advisory Board Member for Merck and GSK.